
About Us
Telemedicine is transforming healthcare, and the demand for feature-rich telemedicine apps is skyrocketing. With the market set to grow from $124 billion in 2026 to $532 billion by 2034, understanding the must-have features is critical for anyone involved in healthcare app development or investing in telehealth solutions.
As telemedicine accounts for 25-30% of U.S. medical visits by 2026, your app must be scalable, secure, and user-friendly. In this post, we’ll break down the essential telemedicine app features and explore advanced tech like AI and machine learning to scale your platform.
Core Patient Features:
Core Provider Features:
Advanced Tech Integration:
Ready to tap into the growing telemedicine market? Start developing your feature-rich app with the essential features that drive success and scalability.
When building a telemedicine app, certain features are non-negotiable. These essential elements form the backbone of a successful platform that meets both regulatory standards and user expectations. As healthcare software development trends evolve, the need for innovative solutions and new technologies becomes increasingly important in ensuring a seamless user experience and operational efficiency.
Here’s a breakdown of the must-have features and how they drive both user satisfaction and operational success:
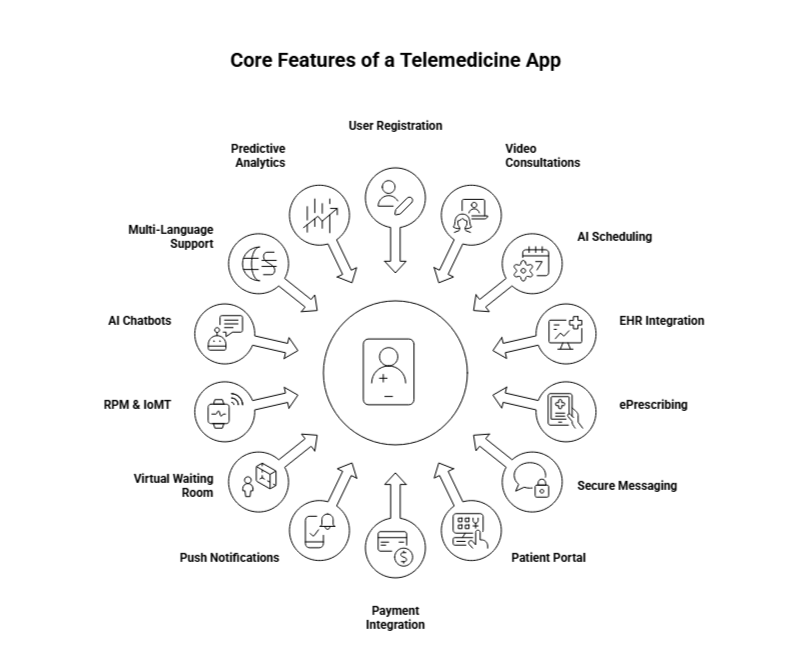
For example, the Bradley County & Cleveland City Schools telemedicine program demonstrated how robust profile management and secure registration can dramatically improve healthcare access. By implementing school-based telemedicine across 27 schools, the districts saw a 1,365% increase in virtual visits, helping students receive care within minutes and eliminating transportation barriers.
Telemedicine apps like Atrium Health’s Hospital-at-Home Program demonstrate how combining video consultations with in-person care and remote monitoring can improve patient outcomes and lower hospital costs, while still providing high-quality care outside traditional settings.
By reducing administrative tasks and improving scheduling flexibility, AI-powered systems can significantly enhance operational efficiency and patient experience, driving long-term value for telemedicine providers.
By integrating EHR, telemedicine apps ensure providers can make informed decisions quickly, ultimately improving care continuity and patient satisfaction. Ochsner Health’s Connected MOM Program, for example, leverages EHR integration for remote monitoring of pregnant patients, improving maternal health outcomes and providing easier access to care for underserved populations.
By simplifying prescription management, telemedicine platforms help reduce bottlenecks in patient care, leading to faster recovery times and fewer administrative errors.
An encrypted messaging system allows for improved access to healthcare information without patients needing to visit the clinic, especially useful for non-urgent follow-ups and routine consultations.
By providing easy access to medical records, patients become more involved in their healthcare, improving outcomes and patient satisfaction. The Mayo Clinic’s virtual care system is a great example of this, offering patients 24/7 access to their health data.
This feature also helps healthcare providers ensure they are compensated for their services efficiently, making the overall system more financially sustainable.
The implementation of such reminders has shown to improve appointment attendance by over 30%, boosting both patient care and clinic revenues.
Virtual waiting rooms have been shown to increase patient satisfaction by up to 23%, providing a seamless bridge between remote consultations and physical healthcare visits.
For instance, Atrium Health’s Hospital-at-Home Program integrates RPM kits to remotely monitor patients, improving patient outcomes and reducing the need for hospital admissions. Additionally, remote patient monitoring is a growing trend: 49% of healthcare professionals cite improved patient outcomes as the top benefit of RPM.
By integrating AI chatbots and symptom checkers, telemedicine platforms enhance patient engagement, reduce wait times, and streamline care delivery.
A study found that only 11% of patient portals are accessible in multiple languages, yet offering this feature could drastically improve patient engagement and outcomes. As the telemedicine industry grows, language support is becoming a key differentiator in reaching broader and more diverse patient populations.
For example, HealthSnap utilizes predictive analytics to assist in chronic disease management, helping healthcare providers predict exacerbations and optimize patient.
Similarly, by anticipating health trends, predictive analytics can help healthcare providers manage population health more effectively, reducing hospitalizations and overall healthcare costs.
Integrating these essential features into your telemedicine app enhances both user experience and operational efficiency. While the telemedicine app development cost may rise with advanced tech like AI, the improved ROI makes it a worthwhile investment. For more insights on building a successful telemedicine platform, refer to our telemedicine app development guide.
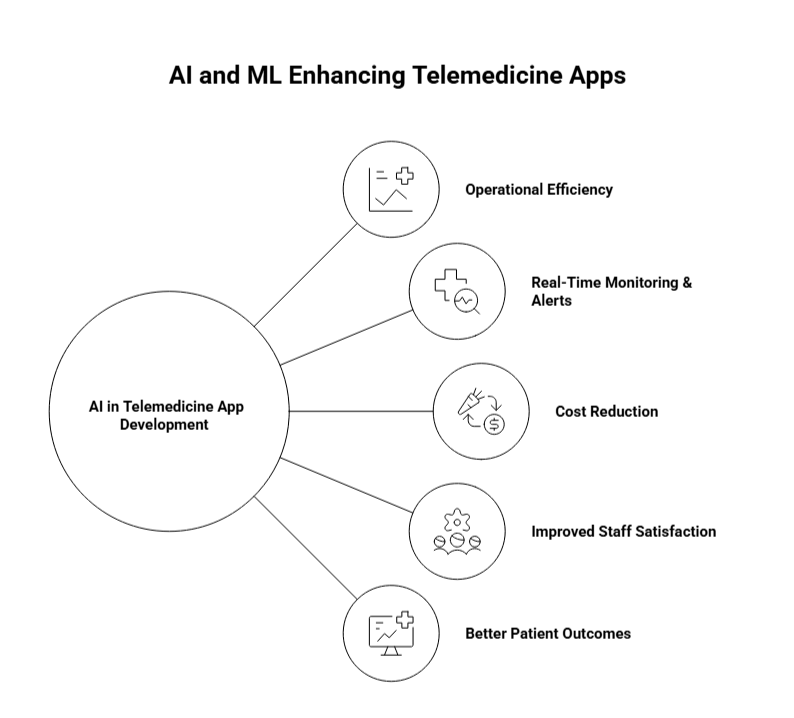
AI and Machine Learning (ML) are revolutionizing the way telemedicine apps operate, enhancing diagnostic capabilities, optimizing workflows, and improving patient outcomes. Here’s how integrating AI and ML can elevate your telemedicine app:
AI’s ability to analyze large datasets and identify patterns far exceeds human capabilities, making it a game-changer in diagnostics. By integrating AI, telemedicine apps can improve the diagnostic accuracy of healthcare providers, helping them detect conditions that may otherwise go unnoticed.
AI’s ability to enhance diagnostic accuracy not only improves patient outcomes but also reduces costly medical errors, making healthcare both more affordable and reliable. It is transforming telemedicine by offering more accurate diagnoses and quicker interventions, ultimately improving patient survival rates and the quality of care.
AI’s role in Clinical Decision Support (CDS) is crucial for real-time, data-driven decision-making. By utilizing AI-powered tools, healthcare providers can make informed decisions based on comprehensive patient data and evidence-based guidelines, all at their fingertips.
By aiding in clinical decisions, AI helps healthcare providers stay up-to-date with the latest medical research, reducing diagnostic errors and improving treatment accuracy. For telemedicine apps, AI-driven decision support ensures that healthcare providers have the right information to deliver the best possible care, even from a distance.
AI and Machine Learning aren’t just for patient care, they also optimize the administrative aspects of healthcare. These technologies automate mundane tasks, from appointment scheduling to medical billing, freeing up staff to focus on what truly matters: patient care.
AI and ML integration have led to a 50% reduction in administrative costs in some hospitals. This not only boosts the bottom line but also improves staff satisfaction and reduces burnout.
By enhancing workflow automation, AI in telemedicine apps increases efficiency, reduces costs, and minimizes administrative errors, leading to a smoother, more streamlined healthcare delivery.
AI’s capability to provide real-time monitoring and alerts is a major benefit in telemedicine. Using AI-powered sensors, telemedicine apps can continuously track a patient’s health data and instantly alert healthcare providers if any critical signs are detected.
In remote patient monitoring (RPM), AI-driven real-time monitoring has been linked to fewer hospitalizations, shorter hospital stays, and reduced mortality rates. AI in telemedicine apps ensures critical findings are flagged immediately, allowing healthcare teams to take swift action, which is key to improving patient survival and long-term health.
However, integrating AI and ML into telemedicine apps can impact the healthcare app development cost, particularly due to the advanced technologies and expertise required. While the initial investment in building AI-powered features may be higher, the long-term return on investment (ROI) can be substantial. AI and ML not only improve patient care and streamline operations, but they also reduce costs by preventing medical errors, improving diagnostic accuracy, and optimizing workflows.
Enhance your telemedicine platform with AI-powered features like predictive analytics, real-time monitoring, and personalized decision support.
HIPAA compliance is a critical aspect of telemedicine, as apps handle sensitive patient data that must be protected to maintain trust and meet legal requirements. With data breaches in healthcare costing an average of $6.45 million per incident, robust security measures are essential for protecting patient privacy. However, the healthcare app development cost often includes the need to incorporate advanced security features like encryption and role-based access control to meet HIPAA standards.
Here’s how top telemedicine apps ensure compliance:
In a digital-first healthcare world, HIPAA compliance is not just a legal obligation, it’s a key factor in protecting patient privacy and ensuring data security. By leveraging encryption, RBAC, audit trails, and real-time monitoring, telemedicine platforms can safeguard patient information and minimize the risk of breaches.
Protect patient data and maintain trust by ensuring HIPAA compliance. AppVerticals offers secure, compliant telemedicine solutions tailored to your needs.
Telemedicine is reshaping healthcare, and now is the perfect time to develop a powerful app that meets the demand for seamless, secure, and patient-centric services.
Whether you’re looking to integrate AI, enhance patient engagement, or ensure HIPAA compliance, AppVerticals has the expertise to turn your vision into reality. We offer custom-built telemedicine solutions with cutting-edge features that scale with your needs. Partner with us to build an app that’s both innovative and future-ready.
Don’t miss out on the opportunity to create an innovative telemedicine platform. From EHR integration to secure video consultations, we can help you build a scalable solution.
Startups often prefer AI-powered tools for efficiency and patient engagement to minimize operational costs. Hospitals, on the other hand, require advanced features like EHR/EMR integration, clinical decision support, and real-time monitoring for managing larger patient volumes and complex healthcare workflows. They also prioritize security features to comply with stringent regulations.
These features protect patient data from unauthorized access and ensure it remains confidential.
Audit trails should also be implemented to track interactions with Protected Health Information (PHI). Moreover, telemedicine apps must have user authentication (multi-factor authentication) and continuous monitoring for potential security breaches to safeguard sensitive data.
AI-powered tools can also aid in image analysis, helping identify diseases like cancer with greater precision. Studies show that AI can achieve 94% diagnostic accuracy in detecting early-stage breast cancer, which far exceeds human capability. AI also assists in clinical decision support, offering real-time, data-driven recommendations for healthcare providers.
Patient portals that allow easy access to medical records, lab results, and prescriptions empower patients to take charge of their health. Additionally, AI-powered symptom checkers and virtual follow-ups create a more interactive and responsive patient experience, leading to higher engagement and satisfaction.
For a seamless user experience, the app should include intuitive navigation, video consultations, appointment scheduling, and patient profile management. EHR integration ensures that healthcare providers can access patient histories easily, improving care quality. Combining security and ease of use is critical to both patient trust and effective healthcare delivery.
Discover how our team can help you transform your ideas into powerful Tech experiences.